I have often come across claims that wish to contest the existence of herd immunity. I find these puzzling. First of all, they are usually offered without proof. But mostly what befuddles me is that the argument approaches the topic backwards. It starts at the wrong end. Let me explain.
Herd immunity, also known as community immunity, is a population-scale name for a phenomenon in the context of disease that can be passed from person to person, and it follows from two factors: vaccine efficacy and vaccination rate. Firstly, vaccines convey immunity to disease. Immunised individuals have antibodies that will neutralise germs when they come in contact with them, making it much less likely to pass on to others – people who are immune don’t get sick and don’t spread the disease. Secondly, if nearly everyone is immune, then almost no one will spread the disease. Thus, even people who have not been vaccinated (and those whose vaccinations have become weakened or whose vaccines aren’t fully effective) often can be shielded by the herd immunity because vaccinated people around them are not getting sick. Herd immunity is more effective as the percentage of people vaccinated increases. For more, see the World Health Organisation on herd immunity.
The vaccination rate that is critical for stopping the spread of disease depends on how infectious the disease is. For measles for instance, which is highly contagious, approximately 95% of the people in the community must be protected by a vaccine to achieve sufficient herd immunity. You can watch a great animation of measles infection spread in populations with different vaccination rates over at The Guardian: Watch how the measles outbreak spreads when kids get vaccinated – and when they don’t. For Hib in Gambia and Navajo populations on the other hand, less than 70% vaccine coverage was sufficient to eliminate the disease, as reported by the WHO.
People who are not immunized increase the chance that they and others will get the disease. It is important to note that there will always be some people who rely on herd immunity rather than individual immunity to stop disease, such as:
- People without a fully-working immune system, like those without a working spleen
- People on chemotherapy treatment whose immune system is weakened
- People with HIV
- Newborn babies who are too young to be vaccinated
- Elderly people
- Many of those who are very ill in hospital
The math of herd immunity
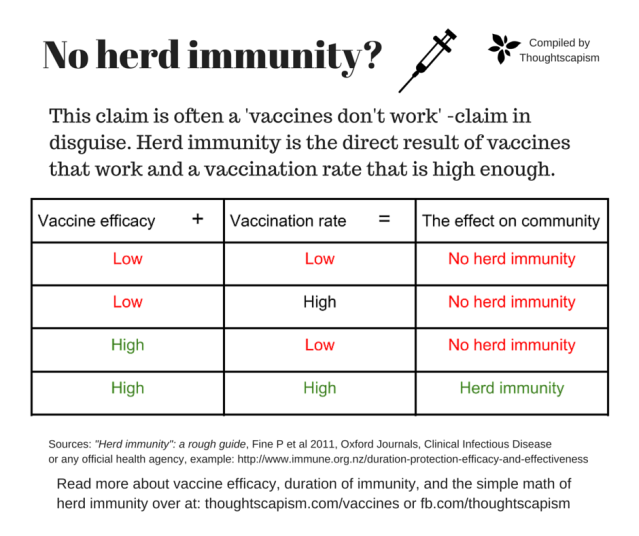
The simple math of the concepts for herd immunity is this: vaccines make people immune + majority of people are vaccinated = community is protected from the spread of disease.
Saying “there is no herd immunity” or “herd immunity does not work” is a roundabout way of saying either that “vaccines don’t protect from disease” or “vaccination rates are not high enough”. That would be a better way of starting the discussion. Then we (and the claimant) would directly know what they were in fact talking about.
When a disease incident occurs, of the kind of infectious disease which (in the absence of immunity) can be passed from person to person, then the situation can be analysed with the four scenarios presented in the table above.
For anyone interested in the the finer details of the real math and biology behind herd immunity, you can read “Herd Immunity”: the rough guide published in the journal of Clinical Infectious disease, or Wikipedia on the mathematics of mass vaccination. I’ll just mention that the necessary vaccination coverage is calculated with the so called reproduction number (R0) of the particular disease, a factor simply for how many people will be infected on average by the person with the disease. What is known as the “herd immunity threshold” or “the critical immunisation threshold” (denoted qc) can then be calculated with the reproduction number:
qc = 1 − 1/R0
Calculated this way, qc gives the percentage of fully immune people required to stop the spread of the disease. In real life scenarios, neither disease- nor vaccine-conveyed immunity is ever quite 100%, and this has to be accounted for by introducing the factor E – vaccine efficacy, or the percentage of people who received the vaccine and will be immune. For measles, which has a reproduction number 12 (or 11-18), and when we factor in vaccine efficacy E, which for measles is about 97 %, we get the vaccine coverage (Vc) necessary for herd immunity, (qc), by the following formula:
Vc =qc/E
Vc = (1 – 1/12) / 0.97 = 0.945
In other words, roughly 94.5 % measles vaccine coverage is necessary to stop the spread of measles in a population.
To recap: herd immunity is a direct effect of vaccine efficacy, that is, the fact that vaccines protect against disease. If one wishes to contest herd immunity, it’s not the term “herd immunity” wherein the problem lies. The problem is either with the vaccination rate (as we are seeing in many places) or with vaccine-induced immunity. The claim of “no herd immunity” really is this: “vaccines do not prevent disease”. This, already, is a more useful starting point for the discussion. All we have to do is look at the evidence – do vaccines prevent the disease they are meant to prevent, and how well?
Vaccines work
There is an incredibly informative site that has graphs (with sources to the raw data) that illustrate the effects on population level of the introduction of vaccines against measles, polio, diphtheria, pertussis, Hib, and Hep B in the United States as well as in the United Kingdom. Please take a look at their great graphs. I’ll only include one here – a graph of measles vaccine introduction in England and Wales. This graph I find particularly interesting because it shows an effect similar to one known in research as the “dose-response” relationship – a very robust method of determining causality.
The change illustrated by this data isn’t a one-time occurrence, a single time-point at which the vaccine was introduced and the disease disappeared simultaneously – for many vaccines, where vaccine coverage was efficient from the start (people were eager to make sure they got their shots as soon as they got available) the disease disappeared rapidly. Instead, here we can follow the effect of gradually increasing vaccination rates (the dotted line), and see that the more people that got the vaccine, the fewer the cases of measles. The graph also shows the dip in the vaccination rates, as they venture below 90% soon after Mr Wakefield began fuelling the fears of the anti-vaccine campaigners around the beginning of the century. The resulting epidemics in the UK have so far only reached over a thousand cases per season, and are thus luckily but a slight bump at the end of the red curve:
Here a comment from federal health resource site vaccine.gov in the same context:
If the drop in disease were due to hygiene and sanitation, you would expect all diseases to start going away at about the same time. But if you were to look at the graph for polio, for example, you would see the number of cases start to drop around 1955 – the year the first polio vaccine was licensed. If you look at the graph for Hib, the number drops around 1990, for pneumococcal disease around 2000 — corresponding to the introduction of vaccines for those diseases.
Again, you can find all the individual graphs for different vaccines in the link where the measles graph came from, here. In addition to the demonstrative disease prevention data from when standard childhood vaccines have been adopted, you can also find scientific publications that have reported specifically on this naturally following result of vaccine efficacy – the herd immunity. Here a study that shows the herd immunity effect with increased protection of unvaccinated populations after introduction of the rotavirus vaccine, for instance. The same is true for the varicella vaccine that protects from chicken pox, excerpt from a study:
Varicella incidence, hospitalizations, and outbreaks in 2 active surveillance areas declined substantially during the first 5 years of the 2-dose varicella vaccination program. Declines in incidence across all ages, including infants who are not eligible for varicella vaccination, and adults, in whom vaccination levels are low, provide evidence of the benefit of high levels of immunity in the population.
Despite all this data some people still feel cheated by vaccines. They claim that vaccines do not deliver as promised, because vaccine induced immunity wanes with time. What’s the deal with that? Let’s look at it next.
So what about waning immunity? Vaccine-induced vs “natural”?
Are vaccines in fact a “fraud” if immunity against diseases can decrease over time? If you approach the question from the perspective of our natural immunity, this isn’t a “fault” of vaccines, no more than it is a “fault” of the diseases themselves when surviving them does not provide a life-long immunity. In fact, natural immunity does not necessarily provide longer-lasting protection than does a vaccine, as found in this study:
A review of the published data on duration of immunity reveals estimates that infection-acquired immunity against pertussis disease wanes after 4-20 years and protective immunity after vaccination wanes after 4-12 years. Further research into the rate of waning of vaccine-acquired immunity will help determine the optimal timing and frequency of booster immunizations and their role in pertussis control.
It is a common trend for an immunity to a disease to wane over a few years or decades. There are things we can do to achieve a longer lasting immunity – like using adjuvants that allow for a stronger immune reaction at the time of vaccination. For some diseases, booster shots may be necessary. Waning immunity is not a “fault” of neither, the diseases nor the vaccines, it is no more or less than a facet of our immune system.
Thanks to vaccines we can harness our body’s natural reaction to pathogens. Our bodies need information about which threats they should protect us from. With remarkably little side-effects, vaccines manage that great feat of delivering that information, of creating immunity, which, before vaccines, was not possible without first enduring the risk of death and disability (at least once). Back then, being in the lucky group – those who would not need to worry about the next wave of disease – may have been a bleak consolation in comparison to the worry of not knowing which of your siblings, friends and relatives would not survive the next ‘immunisation round’.
For more information on the durations of the vaccine induced immunity of our current vaccines, the New Zealand Immunisation Advisory Centre (IMAC) of The University of Auckland have put together a page with an overview of factors that affect vaccine induced immunity and an informative table summary:
Sadly, it appears to me that talking about herd immunity instead of vaccine efficacy may be an (intentional or) unintentional way of obfuscating the topic – an argument about herd immunity may puzzle the discussion participants and it may not be as clear which kind of evidence we should be turning to in order to get to the bottom of the claim. I think many parents searching for information can become confused by similar claims, and, not easily finding a direct answer, may begin to fear the perceived uncertainties in the vaccine debate. With this blog post I wanted to help clarify the concept.
The most important thing to keep in mind, is that while individual arguments may easily seem convoluted and discussions can feel confusing, the discussion of real importance *from the point of view of the evidence*, is the one conducted in the form of scientific publications. So far all the scientific evidence indicates that risks from vaccines are several orders of magnitude lower than the risks from the diseases themselves – in other words, there is a scientific consensus on vaccine safety. If a body of scientific papers should demonstrate a dramatically lowered efficacy of a vaccine, or a substantial risk for harm from a vaccine, we should all take heed. Note that should such an effect be found, they would be the top-ranking news in the scientific community, and anyone reporting such results (should they turn out robust and confirmable by other studies) would be at the high point of their scientist’s career. No amount of coercion or conspiracy could keep the lid on that kind of knowledge. Being a scientist isn’t a glorious occupation, it’s a tough and relatively poorly paying one. Scientists certainly aren’t evil. They are people just like you and me. Scientists love knowledge and understanding of the natural world above all else, that’s why they’re doing what they’re doing.
To quote the summary on herd immunity by L. Shaka, a parent who used to run a site for information on vaccines:
So how do we know that herd immunity exists? First and foremost, if one accepts that vaccines are effective in stopping disease, it is an inevitable logical conclusion. If many, many people are immune the disease will not spread too far. Those that are not vaccinated, and are surrounded by a wall of immune people, will most likely not be exposed to the virus as the spread will stop before reaching them.
Secondly, we can show mathematically how to calculate the herd immunity threshold, by taking into account well established concepts such as the basic reproduction number of the disease.
…
To sum it up the idea of herd immunity is biologically plausible, makes sense logically, can be mathematically modeled based on uncontroversial factors and simple algebra, and is supported by scientific observations and studies.
In other words, to deny herd immunity is to deny biology, logic, common sense, math and science, all in one swoop.
I will round off this post with one last graphic from vaccines.gov, illustrating the effect of vaccine efficacy in a population – a.k.a. herd immunity.

You can continue here if you’d like to read more about: Vaccines and Health. If you would like to discuss the topic below, you are very welcome, but please take note of my Commenting policy.
In a nutshell:
- Be respectful.
- Back up your claims with evidence.





Pingback: Myth: no studies compare the health of unvaccinated and vaccinated people | Thoughtscapism
” In real life scenarios, neither disease- nor vaccine-conveyed immunity is never quite 100%,” should read ” In real life scenarios, neither disease- nor vaccine-conveyed immunity is ever quite 100%,”. By using ‘never’ instead of ‘ever’ you have reversed the meaning of your sentence.
LikeLike
Thanks for pointing out the mishap!
LikeLike
Your chart only starts at 1940 if it went back further your readers would see earlier drops in disease that you fail to mention, and which you wouldn’t be able to explain away with the introduction of vaccines
LikeLike
Hello Lorraine!
Thanks for your interest in my blog. If you click on the link to the collection of disease prevalence graphs, you can find a number of collections that go all the way to 1910, 1912, 1922, and so on. For your convenience, here it is once more: https://medium.com/@visualvaccines/graphic-proof-that-vaccines-work-with-sources-61c199429c8c?hc_location=ufi#.vfp6kr3em
While measles, which my example graph showed, has been somewhat constant in prevalence in the US through 1910-1940, better hospital care did help alleviate the worst effects (unfortunately complications such as encephalitis, deafness do still occur) and was able to save more people, as the death rate from the disease fell somewhat alongside with the advancement of modern medicine (now measles death rate is only about 1 per thousand infected). Unfortunately, before the vaccine nothing had been able to stop the infection of several hundreds of thousands of people (mostly children) every year. I am very happy that I don’t have to live with the dread of these diseases hanging over my head – both through generally higher level of modern medicine care and especially thanks to vaccines – now that I have children.
I hope you found my answer helpful.
Thanks for stopping by!
Iida/Thoughtscapism
LikeLike
The CDC estimates that virtually the entire cohort of children got measles before the vaccine was introduced in 1963. That’s about 4 million live births.
The average death rate from measles the three years leading up to the vaccine was 450 per year or so.
The current claimed rate of death is 1 in 1000 infections. If that were true, the # of deaths in 1963 would have been 4000.
Thus either the 1 death in 1000 infections is wrong or the vital statistics are wrong.
Which is it?
LikeLike
Hello André,
Thanks for your interest in my blog. If you look at the CDC data, they do estimate that yearly 3-4 million people were infected with measles, but that most of those cases were not reported. Since only a fraction were reported, it is not possible to track the death rates of the whole estimated number of cases.
However, the cases that were reported could be tracked, and those statistics before 1963 are:
“Close to 500,000 cases were reported annually to CDC, resulting in:
48,000 hospitalizations
4,000 cases with encephalitis (brain swelling)
450 to 500 deaths”
500 deaths per 500 000 cases demonstrates a mortality rate of 1 per thousand. https://www.cdc.gov/measles/downloads/measlesdataandstatsslideset.pdf
England and Wales had similar data, showing about 2 mortalities per 1000 before 1950s, and the death rates drop below one per a thousand in more modern times: https://www.gov.uk/government/publications/measles-deaths-by-age-group-from-1980-to-2013-ons-data/measles-notifications-and-deaths-in-england-and-wales-1940-to-2013
Thus the vital statistics are reported correctly. Based on what we know about the reported half a million cases annually in the US, and the estimate of the total number of measles cases per year being 3-4 million, the real death rate estimate could indeed be 3000-4000 per year. The cases that were not reported may also be more commonly occurring among the parts of the population who may have been worse off otherwise, and their death rates might have been higher.
The WHO still estimates that: “In populations with high levels of malnutrition and a lack of adequate health care, up to 10% of measles cases result in death. ” http://www.who.int/mediacentre/factsheets/fs286/en/
Other interesting statistic about measles and mortality rates, is that after measles vaccinations, all cause mortalities dropped as well:
“Back in the 1960s, the U.S. started vaccinating kids for measles. As expected, children stopped getting measles.
But something else happened.
Childhood deaths from all infectious diseases plummeted. Even deaths from diseases like pneumonia and diarrhea were cut by half.”
…
“So it’s really been a mystery — why do children stop dying at such high rates from all these different infections following introduction of the measles vaccine,” he says.
…
“We found measles predisposes children to all other infectious diseases for up to a few years,” Mina says.” http://www.npr.org/sections/goatsandsoda/2015/05/07/404963436/scientists-crack-a-50-year-old-mystery-about-the-measles-vaccine
Monkey studies so far have indicated that measles may give a sort of ‘immune amnesia’ – it wipes away the immunities already acquired to other diseases, making children susceptible to them as well, again.
Nasty disease, all in all.
Hope you found my answer helpful. Thanks for stopping by!
Iida/Thoughtscapism
LikeLike
Hi, Iida.
It doesn’t make sense to use just the reported cases without disclosing that it is just the reported case rate. That’s leaving out the most important part of the story.
A more rigorous and correct way to say it would be, “The death rate among reported cases is 1 in 1000. However, not all cases were reported and typically only the worst cases were hospitalized and then subsequently died. Given that the CDC estimates the entire cohort of children got the measles, say 4 000 000 cases, the true death rate is closer to 450 / 4 000 000 or 0.01125%.”
LikeLike
Hello Andre,
It isn’t correct to report death rate as lower than it actually is. CDC reports death rate for the cases that they have actually followed, the rest are up to estimates. You seem to estimate that there were no deaths among untracked cases, but that is based on an assumption you make. You would need some data to back that up.
LikeLike
Also, do you have a link to the monkey studies in this comment?
“Monkey studies so far have indicated that measles may give a sort of ‘immune amnesia’ – it wipes away the immunities already acquired to other diseases, making children susceptible to them as well, again.”
My understanding was that Mina’s study was entirely theoretical.
LikeLike
The Minas study tracked real world incidence of measles and other infectious disease, and looked which model could explain the patterns.
Here is a monkey study: Measles Immune Suppression: Lessons from the Macaque Model
“Measles remains a significant childhood disease, and is associated with a transient immune suppression. Paradoxically, measles virus (MV) infection also induces robust MV-specific immune responses. Current hypotheses for the mechanism underlying measles immune suppression focus on functional impairment of lymphocytes or antigen-presenting cells, caused by infection with or exposure to MV.”
” Our findings indicate an immune-mediated clearance of MV-infected CD45RA− memory T-lymphocytes and follicular B-lymphocytes, which causes temporary immunological amnesia. The rapid oligoclonal expansion of MV-specific lymphocytes and bystander cells masks this depletion, explaining the short duration of measles lymphopenia yet long duration of immune suppression.”
http://journals.plos.org/plospathogens/article?id=10.1371/journal.ppat.1002885
And here’s an earlier review of measles immuno supression mechanisms: https://www.ncbi.nlm.nih.gov/pubmed/20636817
LikeLike
“It isn’t correct to report death rate as lower than it actually is. ”
If it isn’t correct to report the death rate as lower than it actually is then it isn’t correct to report the death rate higher than it actually is.
The statement should read, “The lower bound of the death rate is 0.01125% and the upper bound is 1 in 1000. The likely number is closer to the lower bound since most cases of measles are mild.”
Saying that the actual death rate is 1 in 1000 cases is not accurate even a little bit.
LikeLike
The death rate of 1 in 1000 is accurate based on the very large data sets available. It has been confirmed by the measles statistics from other countries as well. If you have evidence of a different data set, where death rates are lower, then you may present that. Hypothetical ideas of what death rates may have been in other data sets, however, do not qualify as evidence.
LikeLike
The data set is clearly incomplete, as the CDC itself states, and a note to that effect should accompany any statistics derived from that.
Are the data you say support the 1 in 1000 number from developed or developing countries?
LikeLike
I have provided it. Please read my comments and follow the sources. Disease statistics are useful and accurate if their sample is large an representative enough. Modern meticulous disease tracking of complete countries’ populations has not been available for most of history, or most of the world, but the data of hundreds of thousands of cases, that has been collected, is the best evidence we have to go on.
If you keep claiming that the evidence above is not accurate, over and over again, based on no actual evidence of the contrary, this discussion will no longer serve a purpose.
Hope you enjoy your day, thanks for interest in my piece.
Iida/Thoughtscapism
LikeLike
Then why is it that most people catching the mumps, and all of the Disney Land measles cases were people that were vaccinated? Do we chalk this up to ineffective vaccines?
LikeLike
Hello Emma,
Thanks for stopping by! Sorry that you had to wait so long for a reply, I have been taking a couple of months break from the internet. Before you continue, however, please read my commenting policy: https://thoughtscapism.com/about/commenting-policy/ Claims in the comments section of this blog should be backed up with evidence. For instance, if you had taken the time to look at the actual Disney Land measles epidemic data, you would have very quickly learned that vaccinated people were among the minority, only 1 % of the infected having confirmed to have had all three doses. This is remarkable, considering that the vaccinated vastly outnumber the unvaccinated among the people exposed.
“Among the 110 California patients, 49 (45%) were unvaccinated; five (5%) had 1 dose of measles-containing vaccine, seven (6%) had 2 doses, one (1%) had 3 doses, 47 (43%) had unknown or undocumented vaccination status, and one (1%) had immunoglobulin G seropositivity documented, which indicates prior vaccination or measles infection at an undetermined time. Twelve of the unvaccinated patients were infants too young to be vaccinated. Among the 37 remaining vaccine-eligible patients, 28 (67%) were intentionally unvaccinated because of personal beliefs, and one was on an alternative plan for vaccination. Among the 28 intentionally unvaccinated patients, 18 were children (aged <18 years), and 10 were adults." https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6406a5.htm?s_cid=mm6406a5_w
Here an example with MUMPS, to explain the normal situation, where many vaccinated people, and just a few unvaccinated (as they are generally in stark minority) are exposed to a disease. The percentage of infected is always much much higher among the unvaccinated, while generally only a few percent of the vaccinated have the bad luck of catching the disease. That few percent might still be many people – as many or more than the total number of unvaccinated that get sick. But that little percentage among the vaccinated is nothing compared to how many of them would have caught the disease had none of them been vaccinated:
"Vaccination and Mumps Outbreak: an Example
"Example: Let’s say that an outbreak occurs among 1,000 people and that 950 of these 1,000 people have received two doses of the vaccine and 50 are unvaccinated (i.e., vaccine coverage is 95%). If there is a 30% attack rate among people who haven’t been vaccinated, 15 unvaccinated people would get the disease. Among the 950 vaccinated people, the attack rate would be 3%, so 29 vaccinated people would get the disease. Therefore, of the 44 people who got sick during the outbreak, the majority (29, or 66%) would have been vaccinated. This doesn’t imply that the vaccine didn’t work. In fact, the people who hadn’t been vaccinated were 10 times more likely to get sick as those who had been vaccinated, it’s just that there were a lot fewer unvaccinated people at risk. Furthermore, if none of the 1,000 people had been vaccinated, the outbreak would have resulted in 300 cases rather than only 44. In this scenario, we would say that the vaccine is 90% effective in preventing the disease after two doses, which is the same as saying that the attack rate in the unvaccinated group is 10 times higher than the attack rate among people who have received two doses of vaccine. The formula to calculate vaccine effectiveness is (attack rate in unvaccinated group minus attack rate in vaccinated group) divided by attack rate in unvaccinated group, or (ARU-ARV)/ARU." https://www.cdc.gov/mumps/hcp.html
I hope you find the information useful. Thanks for your interest in my blog, hope you have a nice day.
Best regards,
Iida/Thoughtscapism
LikeLike
Pingback: Antivax Myth: “Herd immunity isn't real” - Vaccine F.Y.I.
I wish I had read this before I gave up the fight I was having
regarding vaccines. I gave up when the other side posted an
article stating there is no such thing as herd immunity.
If they didn’t at least accept that premise I knew throwing
all the science I had at them wasn’t going to have any affect.
I appreciate your calm and genial responses.
LikeLiked by 1 person
Thanks so much, Ms Mitty!
I know it’s often not easy to talk about this with people who really feel afraid of vaccines. Good on you for giving it a shot. It doesn’t always accomplish anything, but then again, sometimes it might!
Appreciate you dropping me a line 🙂 Hope you have a great day,
Iida/Thoughtscapism
LikeLike
Hi. While I don’t dispute the end result of vaccines I do wonder if it would take days for vaccine produced anti bodies to fight off the antigens. Would this not change the calculation for herd immunity.
LikeLike
Hello Philip,
Herd immunity is a field of science that includes many complicated variables. Among the biggest variables are considered to be R0, or the reproduction number – how many people a sick person infects – and the heterogenity of populations, that is, they include pockets of unvaccinated vs vaccinated people, instead of a homogenous mix. But there is a lot more to it as well, if you are interested, this article goes in depth to the theory and practice of herd immunity: Herd Immunity: History, Theory, Practice http://www.assis.it/wp-content/uploads/2016/01/crude-herd-immunity.pdf
From their discussion: “Much of the literature on herd immunity to various infections emphasizes the estimation of theoretical threshold proportions of immunes which, if reached and sustained (e.g., by vaccination), should supposedly lead to progressive elimination of the infection from the population. Such estimates provide a rough ranking of the probable levels of natural and vaccine-derived immunity required for eradication of these infections.
…
Even if the goal is eradication, the practical approach will not be to just attain some threshold and sustain it, but to aim for and sustain the highest possible coverage, in theory 100 percent, as this will maximize the rapidity of the disappearance of the infection in question. Merely achieving a herd immunity threshold does not mean immediate disappearance of the infection, it only starts a downward trend.”
In contrast, the time a vaccinated person may be fighting off the infection is not considered a significant factor in the context, because of how greatly vaccines reduce the chance of transmission. Some vaccines protect even against infection (eliminating even the potential for transmission), while most others are effective enough to fight off the infection without giving the pathogen enough time and reproduction opportunities in the body to cause spread in practice. From the WHO:
“Many vaccines are primarily intended to prevent disease and do not necessarily protect against infection. Some vaccines protect against infection as well. Hepatitis A vaccine has been shown to be equally efficacious (over 90% protection) against symptomatic disease and asymptomatic infections.26 Complete prevention of persistent vaccine-type infection has been demonstrated for human papillomavirus (HPV) vaccine.27 Such protection is referred to as “sterilizing immunity”. Sterilizing immunity may wane in the long term, but protection against disease usually persists because immune memory minimizes the consequences of infection.28”
…
“The decline of disease incidence is greater than the proportion of individuals immunized because vaccination reduces the spread of an infectious agent by reducing the amount and/or duration of pathogen shedding by vaccinees,34 retarding transmission.” http://www.who.int/bulletin/volumes/86/2/07-040089/en/
Hope you find these sources useful.
Have a great day,
Iida/Thoughtscapism
LikeLike
Pingback: Seven Reasons Why You Really Don’t Want to Have Measles | Thoughtscapism
Thanks for your clear, succinct, reasoned and unemotional article. I have pointed many people to it for reference. Thanks for maintaining it all this time. It is such a shame that it is still needed in this day and age. Ireland has just today put out a warning that the vaccination rate for measles has dropped to 92% below their 95% target.
LikeLike
Hello Pól,
Thank you very much for your kind comment. It means a lot to get positive feed back! I am happy that you find the piece useful. I’m very sorry to hear that there is a dip in vaccination rates in Ireland as well Seeing as measles is spreading far and wide in Romania, Italy, Germany, France, UK, and Switzerland at the moment, perhaps the news will alert more parents into catching up with their kids vaccinations.
Seeing as measles is spreading far and wide in Romania, Italy, Germany, France, UK, and Switzerland at the moment, perhaps the news will alert more parents into catching up with their kids vaccinations.
All the best,
Iida/Thoughtscapism
LikeLike
One line in my textbook has always bewildered me and trying to find more about it brought me here
“Herd effect is less pronounced for vaccines that protect only against disease eg. diphtheria than those that prevent infection eg. measles, opv ”
Should I understand from this line that disease and infection are not same, as diphtheria disease might cause clinical infection by releasing exotoxin which is the actual culprit.
LikeLiked by 1 person
Hello! Thanks for stopping by, sorry that I did not have time to respond earlier.
We actually touched on this on a comment just a bit above your question. This might be helpful:
“Many vaccines are primarily intended to prevent disease and do not necessarily protect against infection. Some vaccines protect against infection as well. Hepatitis A vaccine has been shown to be equally efficacious (over 90% protection) against symptomatic disease and asymptomatic infections.26 Complete prevention of persistent vaccine-type infection has been demonstrated for human papillomavirus (HPV) vaccine.27 Such protection is referred to as “sterilizing immunity”. Sterilizing immunity may wane in the long term, but protection against disease usually persists because immune memory minimizes the consequences of infection.28”
…
“The decline of disease incidence is greater than the proportion of individuals immunized because vaccination reduces the spread of an infectious agent by reducing the amount and/or duration of pathogen shedding by vaccinees,34 retarding transmission.” http://www.who.int/bulletin/volumes/86/2/07-040089/en/
Hope you find the source useful.
Have a great day,
Iida/Thoughtscapism
LikeLike
Pingback: Conversation with an anti-vaxxer… ? – On The Fence About Vaccines
Pingback: How Can the Unvaccinated Spread Diseases They Don’t Have? – VAXOPEDIA
If the duration of immunity is not lifelong then how is it that we don’t see widespread outbreaks of the diseases in adult population? I have not heard of adults getting MMR so wouldn’t they be highly susceptible to Mumps, since it is not expected to last into adulthood? Tdap rates for adults are 23% which would make that population not immune. https://www.cdc.gov/vaccines/imz-managers/coverage/adultvaxview/coverage-estimates/2015.html Tetanus, diphtheria, and pertussis immunity doesn’t last until adulthood so I struggle with understanding how we can attribute the low incidence of those diseases in the whole population to vaccination and herd immunity. Maybe you can help me understand?
LikeLike
Hello pl101,
Thanks for your interest in my piece. At the point when immunities wane too much, we do get below good herd immunity thresholds and the diseases are once more able to spread, if they are still endemic in the area, or are brought in from another part of the world. Pertussis, for instance, does not have a high enough (booster) vaccination rate and has not been kept entirely in check, as thousands of cases of pertussis still pop up in pockets of vulnerable people in the US. Herd immunity does protect all those who happen to be surrounded by enough people who have had recent enough vaccinations or adult boosters, as for instance recommended extra for all family members of parents with infants – and the current levels of vaccination are why pertussis cases are drastically much lower than before the vaccines, although not entirely eliminated.
With regards to duration of tetanus and diphteria vaccine immunities, those appear longer than at first estimated. “Mathematical models combining antibody magnitude and duration predict that 95% of the population will remain protected against tetanus and diphtheria for ≥30 years without requiring further booster vaccination.” https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4826453/
Pertussis, to my knowledge, is still shown to wane faster and for optimal protection a booster every ten years is recommended.
Further, how many people need be immune for the effect to remain depends on how infectious the disease is. Measles is very infectious, a sick person infecting on average 12-18 others, whereas pertussis has a reproduction number of 5.5 (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2889930/), so with an effective enough vaccine, a lower portion of the population would be enough to stop the spread.
What CDC data you linked shows, btw, is not precisely how many percent of the adults are still protected by the TDAP vaccine, they just show how large a portion received a booster shot within the last ten years. Studies estimating how long the vaccine protection lasts are varied, and some also indicate a range longer than ten years (one I referenced suggested upper range 12 years). The young generation (roughly a fourth of the population) are generally protected by the vaccinations (the vaccination rate is high); a certain portion of the population may still have immunity from the vaccines after a longer time than ten years past youth or previous boosters; and roughly a fourth of the adult population have received a booster within the last decade. That gives something more than 50% immunity, but probably nowhere near as high as 90%, and it has evidently not been enough to entirely stop the epidemics.
Hope that helped clear it up.
Please don’t hesitate if you have more questions.
Thanks for stopping by,
Iida/Thoughtscapism
LikeLike
Thank you for taking the time to respond.
As I understand it herd immunity is like a critical/threshold value. Below the critical value and the outbreaks are not contained within the non-immune population and above it they are contained to small pockets of individuals without immunity (due to herd immunity protection).
e.g. https://offspring.lifehacker.com/%5Bobject%20Object%5D
Pertussis has an estimated threshold of 92-94% (http://sitn.hms.harvard.edu/wp-content/uploads/2010/09/Lecture_1.2.pdf). I don’t think we are past that threshold looking at the whole population.
Therefore, I would expect a high incidence of pertussis in adults but that population has the lowest: https://www.cdc.gov/pertussis/surv-reporting.html
Tetanus is not applicable to herd immunity: https://www.cdc.gov/vaccines/pubs/surv-manual/chpt16-tetanus.html
Diphtheria seems to be virtually eliminated in developed countries and worldwide only thousands of cases are reported (https://www.cdc.gov/diphtheria/clinicians.html) while I would argue that herd immunity levels are not achieved worldwide.
It doesn’t look to me like the math of herd immunity matches actual observations. By the theory, if levels aren’t high enough you don’t have herd immunity and there should be epidemic outbreaks in entire non-immunized population. We don’t have the herd immunity levels of immunization in whole population and yet the incidence is not widespread; we only see small outbreaks.
Also, thank you for the reference to the study on duration of immunity. I can see why the estimates are so varied. Data is sparse at later ages after vaccination and the range for early ages is huge!
LikeLike
Thanks for your interest! Will try to come back with better time later, but this “As I understand it herd immunity is like a critical/threshold value.” Concept is not quite in line with the literature. Herd immunity appears at any level where a particular individual/groups are shielded by only interacting with people who are immune and thus are shielded. The threshold is where disease epidemics are predicted to be extinguished completely on a large population level. Under that, smaller pockets of disease are predicted to erupt, which matches observations quite well. I believe there is some discussion about this in earlier comments in this thread (or perhaps just the previous vaccine piece), as said, I’ll try to come back and add the literature later.
LikeLike
Thank you for the interesting post; you have made great efforts to gather all these information which provide valuable insights into the matter.
Please I wanted to know if you have any idea about the threshold of vaccination that is required to achieve herd immunity for tuberculosis.
Thanks
LikeLike
Hello,
R0*(1-qc) = 1, or qc=1-1/R0 is commonly used in epidemiological literature. The underlying model makes the silent assumption, that an initial “patient zero” P0 is infecting a random stranger P1, and they both won’t meet soon again. However in real life, most people who meet already know each other, and will meet again soon on a regular basis, because they are e.g. family members, classmates, or co-workers. But if someone has infected me, I can’t infect them back when we meet again, since now, after going through the disease, they are naturally immunized.
So we need to distinguish the case that P0 and P1 either know or don’t know each other. For simplicity, lets assume an unvaccinated person always contracts the virus if he meets an infected person. We look at 3 different situations:
Case 1, no acquaintances, only strangers: In a completely unimmunized population, a person P1 is infected accidentially by P0, and in turn P1 is infecting R0 random people, who P1 won’t meet again soon. This is the situation described by the conventional formula qc=1-1/R0.
Case 2, only acquaintances, no strangers: Lets assume a completely unimmunized population, where P1 is in contact with R0 people who he knows and meets on a regular basis, among them P0, who first infects P1, and then P1 in turn infects all the R0-1 other persons who are not immune yet. In order to stop an epidemy, we have to vaccinate enough people to make sure that in average groups of R0 persons, apart from P0, at most one of the reamining R0-1 persons remains unvaccinated:
R0*(1-qc)-1=1 or qc=1-2/R0.
Case 3, where P1 has A acquaintances and also meets S strangers. Then R0=A+S. With probability A/R0, P0 will be an acquaintance of P1, and with probability S/R0, P0 and P1 are strangers. Then the critical immunization rate must meet the condition:
1=[(1-qc)*R0-1]*A/R0 + [(1-qc)*R0]*S/R0, which means
qc=1-1/R0-A/(R0*R0) or qc=1-2/R0+S/(R0*R0).
If A=0 and R0=S we get back case 1, and if A=R0 and S=0 wet get back case 2.
Most everyday life situations will resemble case 2, with most contacts happening between people who know each other, and very little contact between strangers, and If we assume again a 97% vaccine efficiency and R0=12 here, we see that Vc=(1-2/13)/97%=87.2% is already a sufficient vaccination rate to stop an epidemy, which means a much smaller vaccination rate will be sufficient than what WHO usually claims.
The Disney theme park outbreak 2014 is just the exception proving the case in point, since much lower measles vaccination rates have been preventing outbreaks in schools and kindergardens where children meet each other every day; while the same vaccination rates could not prevent an outbreak at Disneyland, where most people only meet by random once. Also, from the diagram “Measle Notification in England and Wales”, we can observe that vaccination rates far under 90%, even as low as 80% have been able to prevent epidemies for many year in these countries.
WHO and national governments are saying 95% must be vaccinated. So basically they are using a wrong model and formula, and striving for a far too high vaccination rates. There may be a couple of reasons for this politics: First, in order to decrease disease cases, the real vaccination rate must be somewhere slightly above the critical rate, so using 95% is a practical choice. Then of course higher vaccinatino rates help the pharmaceutical industry to sell more of their products.
The main reason I suspect for choosing a too high vaccination rate is tactical. The simple epidemiological models assume homogenous mixture of vaccinated and unvaccinated people in a population. In reality, homogeneity will never be achieved. The higher vaccination rate of the general population climbs, the more often cases of the disease will remain in particular social groups and classes who stay below critical immunization for some reason. Governments, in order to avoid social unrest and allegations of discrimination, often shun a direct confrontation with these less vaccinated groups. Rather, government prefers to issue laws which try to raise the general vaccination rate further and further, even if this can’t further reduce number of disease cases.
LikeLike